Pain Relief: Federal Agencies Target Patient-Centric Healthcare
The healthcare industry has reached a critical juncture. Today, there is both accessible health data and demand to consume health information that is driving a new wave of federal innovation focused on empowering the patient. While a complete transformation to a patient-centric model in the next five years may be aspirational, government agencies are beginning to invest in three key areas of innovation.
As pain points go, the US health system has plenty for patients and providers alike. If there is to be relief from high costs and low quality in key areas of care, US government healthcare agencies will need to evolve towards a more patient-centric model. This new paradigm will be efficient – saving hundreds of billions of dollars currently spent on doctors’ visits that primarily disseminate information; high impact – dramatically improving care for underserved communities such as the elderly, while more efficiently managing chronic lifestyle diseases; and innovative – leveraging data to radically enhance our collective medical knowledge based on the sophisticated analysis of billions of encounters and outcomes.
While these concepts – efficiency, impact and innovation – are common traits in most sectors, they are rare in government healthcare. The patient experience will become more like the general consumer economy, with everything from provider-comparisons tools offering new levels of choice, accountability and value, to access to and mobile control of personal health information to make informed care decisions from anywhere.
While a full realization of this vision is still far off, there has been a notable shift to address several of these areas within the federal government over the last year. The healthcare industry is at a critical moment where the democratization of information following the Health Information Technology for Economic and Clinical Health (HITECH) Act digitization revolution, and burgeoning demand for healthcare information from the citizen post-Affordable Care Act (ACA) has created an environment ripe for change in the way we manage, distribute and consume health information. Across healthcare agencies, implementation initiatives are driving a new wave of opportunity in federal health.
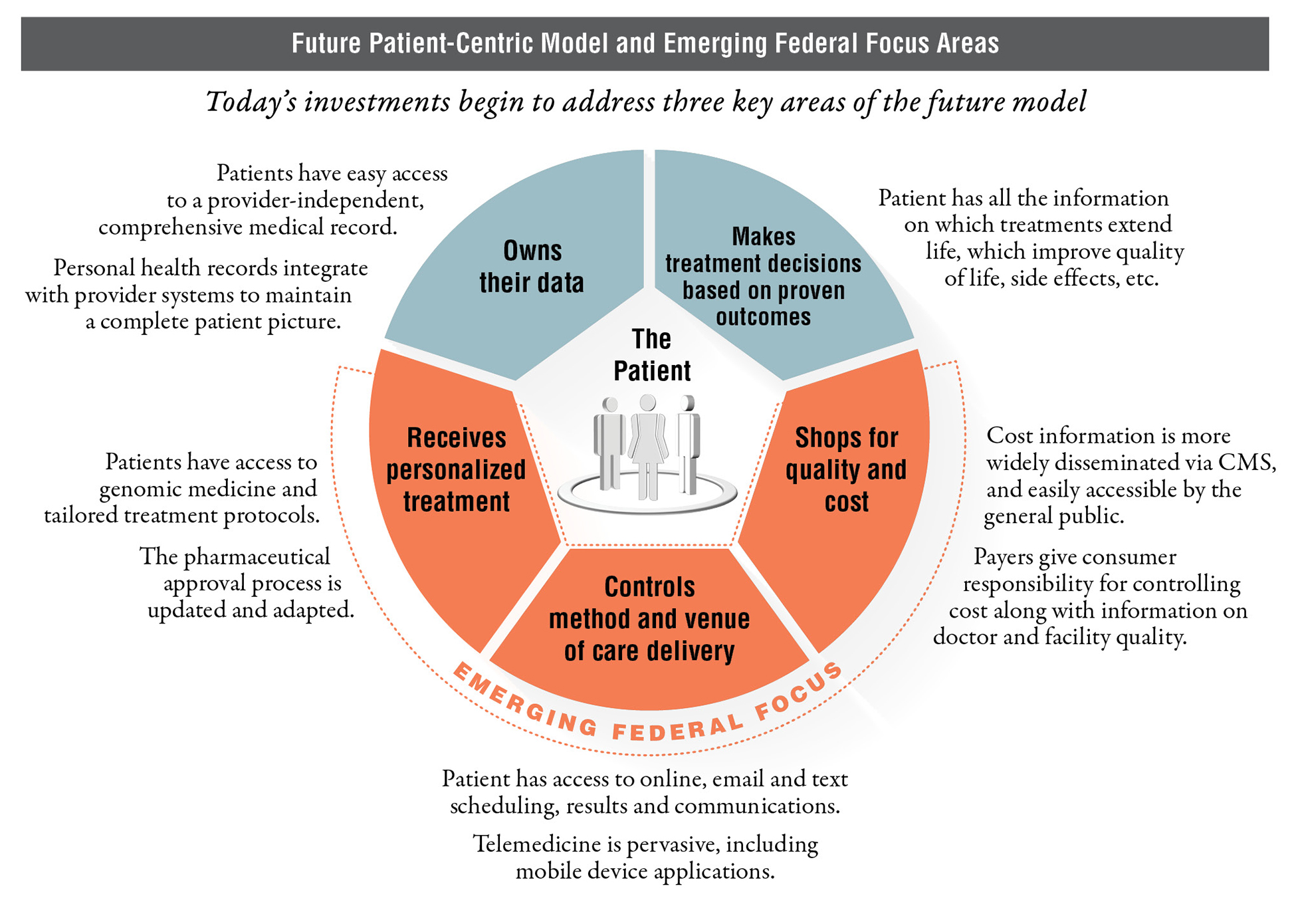
Shops for Quality and Cost – Improving Websites and Decision-Making Tools at the Centers for Medicare and Medicaid Services (CMS): After coming under fire from the Government Accountability Office (GAO) in November, CMS is looking to improve its patient engagement through its healthcare transparency tools, with a focus on websites allowing patients to compare providers. In Secretary Burwell’s February 26, 2015 testimony to Congress, she stated that CMS is “making major strides to expand and improve its provider compare websites, which empower consumers with information to make more informed healthcare decisions, encourage providers to strive for higher levels of quality, and drive overall health system improvement.” With the goal of enabling citizens to act as consumers and incentivizing providers to, in effect, compete for patients, CMS is looking to add new data while increasing information on cost and key differences in quality of care for existing tools. Additionally, once these tools are fully functional, CMS may look to increase its outreach to communicate the full breadth of options for interacting with CMS.
Controls Method and Venue of Care – Rise in Mobile Apps: At a recent innovation awards event, a government speaker explained the need to catch up to commercial industries, stating that innovation is “not about making something totally new, but trying to improve service delivery; we’re not trying to send rockets into space, just trying to do things that the private sector does already.” The official cited the ease of mobile check deposits in the banking world as a successful example of private sector innovation. Agencies are betting heavily on technology to improve patient outcomes and satisfaction, specifically looking to mobile apps. The VA Mobile Health program, for example, is currently working on 16 applications supporting everything from on-the-go veteran’s benefits questions (311VET) to the viewing of personal VA medical information (VA Health Summary of Care). The Military Health System is similarly focused on application development, recently receiving FDA clearance for a mobile app to diagnose head injuries.
Receives Personalized Treatment – Precision Medicine Initiative at HHS: In its FY16 request, the Department of Health and Human Services (HHS) requested $215M for a cross-agency effort, focused on developing treatments, diagnostics, and prevention strategies tailored to individual genetic characteristics. If approved, this funding will provide a significant boost to the National Institutes of Health (NIH, $200M), also adding to the Food and Drug Administration (FDA) and the Office of the National Coordinator for Health IT (ONC), as HHS looks to incorporate genomic data from over 1 million Americans to expand cancer research. This new study also opens the door to future data sharing between the federal and commercial health communities to enable more precision medicine, with projects such as eMERGE out of the National Human Genome Research Institute already setting the stage for linking DNA biorepositories with electronic health record (EHR) systems.
Other Emerging Areas – Improving Provider Communication & Patient Safety: In addition to these areas of focus, the government has begun working closely with commercial health providers to improve patient safety. The Military Health System is leading the way by collaborating with the commercial sector on a new system, I-PASS (Illness severity, Patient summary, Action list, Situational awareness and contingency planning, and Synthesis). I-PASS enables improved communication and team-training tools for the handoff of patient care between providers. Walter Reed National Military Medical Center (WRNMMC) is the first military hospital involved in the study, partnering with nine major children’s hospitals to develop the tool, leading the curriculum adaptation for multiple clinical areas such as adult medicine.
As the government embarks on this transition, it is looking to the health IT industry to help them engage patients and harness the power of the commercial sector. To position for this transformation, federal contractors should:
- Partner with agile, innovative commercial firms to help bring the latest approaches in patient-centric care to the federal environment
- Boost health-specific branding through white papers, pilots and other marketing initiatives to increase visibility with the government customer
- Look to ongoing programs for opportunities to introduce innovation, while positioning your firm as a thought leader within the customer community
- Develop methodologies and intellectual property that the government customer will find compelling – they can’t buy what they can’t even imagine
- Define a clear growth vision for relevant businesses to focus business development resources and other investments
Federal contractors pursuing proactive strategies focused on tomorrow’s healthcare dynamics, not those of today, will have a significant advantage over firms that merely react to the change at hand.





