Telehealth at the Starting Line: COVID-19’s Impact on Telehealth Maturity and Where We Go From Here
Telehealth platforms have far outpaced adoption of telehealth for years, despite investments made across industry to advance and create useful technology.
When the COVID-19 pandemic hit the United States and shelter-in-place orders warned of unnecessary trips outside the home, healthcare providers were forced to rapidly – if not haphazardly – begin to overcome historically challenging barriers to implementing a successful telemedicine system that continues to support patients.
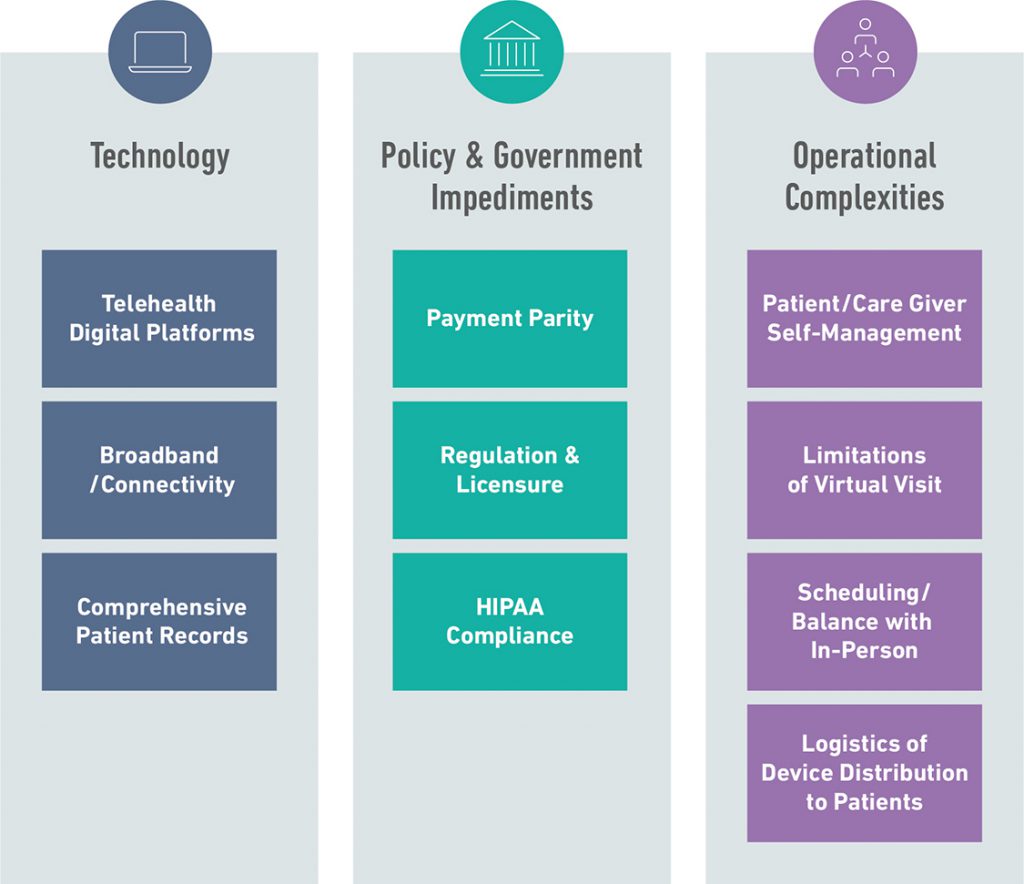
Many of these barriers relate to payment and regulation –
- How should physician licensure apply across states?
- How can we ensure technologies are HIPAA-compliant?
- How do we pay for telehealth services, and does it demand payment parity with in-person visits?
These challenges are further amplified by the lack of data related to telehealth, since it has yet to be adopted at scale for enough time. Without numbers to back up the potential cost savings or health outcome improvements, the value proposition of adopting telehealth for providers remains limited.
Operational complexities also exist surrounding how a provider offers both in-person and telehealth services –
- How should the provider split their time?
- How do you balance on-demand and scheduled telehealth visits?
- How do you ensure you get the appropriate information (i.e., vitals, blood test results, and more) to provide adequate care?
- Which practice areas or specific conditions are telehealth-appropriate?
These challenges remain, but the urgency of finding an appropriate remote care solution during the pandemic created an opportunity to re-think how the U.S. health care system supports telemedicine.
Challenges to Widespread Telehealth Adoption
How Has COVID-19 Changed the Current Telehealth Policy?
The Department of Health and Human Services (HHS) temporarily suspended HIPAA requirements for telehealth technologies in March 2020, paving the way for platforms like Facebook, Google Duo, and Facetime to enter the telehealth scene.
The Trump administration allowed Medicare telehealth visits to be reimbursed at the same rate as in-person visits during this national emergency, as well as audio-only visits that were formerly under greater restrictions.
We saw the President take action through executive order on August 3rd, making permanent many of the temporary flexibilities for telehealth in Medicare. The order also requires HHS to announce a new innovative payment model for rural healthcare, giving providers more flexibility including with virtual health.
Congress continues to introduce legislation to shape the future of telehealth, receiving support from both political sides of the aisle.
Regardless of how the policy shakes out, one thing is clear: Telemedicine – in its many forms – is here to stay. Although we have rapidly overcome many historical barriers, we are just at the starting line of meaningful adoption.
Telehealth Maturity Curve: Challenges of Adoption
Some of the initial hurdles to telehealth were necessary to jump over before a more serious conversation about widespread adoption could even begin. And if the past five months have revealed anything, it is that telehealth is incredibly complicated.
The COVID-19 crisis has enabled us to shift the focus from challenges related to regulation and policy, payment parity, and technology/HIPAA-compliance toward numerous operational complexities brought to light by accelerated telemedicine adoption.
Telehealth Maturity Curve
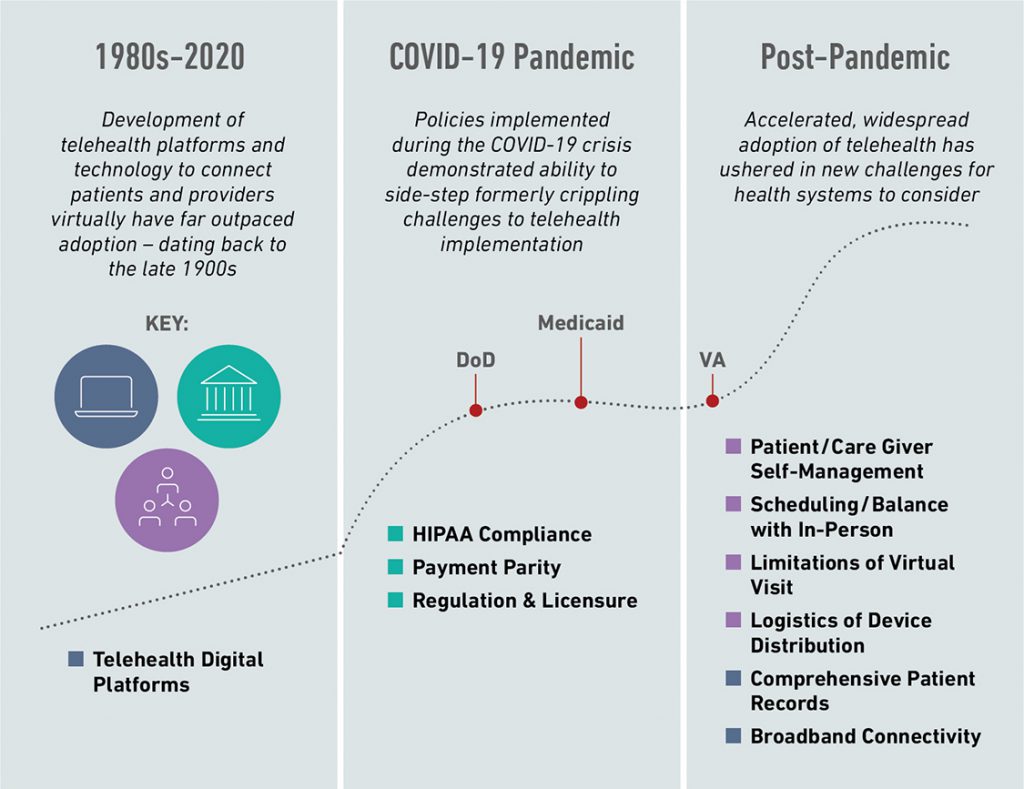
As we move toward a more mature stage of telemedicine, healthcare systems will have to find solutions to these additional challenges:
- Logistics of Device Distribution:
For a telehealth model to be most effective, there is likely a need for patients to have certain medical devices at home to supplement audio/video communication with a medical professional. These remote patient monitoring devices exist, but it is difficult to ensure all beneficiaries have access to these devices in larger, dispersed patient populations. - Access to Broadband Connectivity:
In rural areas of the United States, WiFi or data connectivity can be hard to come by, significantly affecting patients’ access to telehealth in those regions. These patients also tend to suffer due to long distances from their home to the nearest doctor’s office or hospital. - Virtual Visit Limitations:
Phone calls, and even video conferencing, only go so far. Many visits require a physical exam and the collection of health data and/or samples. Some systems have tried to tackle this challenge by purchasing home monitoring devices for beneficiaries. Further, some companies have come forward with a telehealth plus in-home nurse solution. - Scheduling:
Though the pandemic is likely to continue to limit in-person visits in the near-term, eventually providers will have to address the operational complexity of managing a schedule that includes both in-person and virtual visits. - Need for Patient (or Caregiver) Self-Management:
Telehealth puts a substantial burden on a patient, or their caregiver, to manage their care in a way that in-person visits do not require. - Comprehensive Patient Records (and Security):
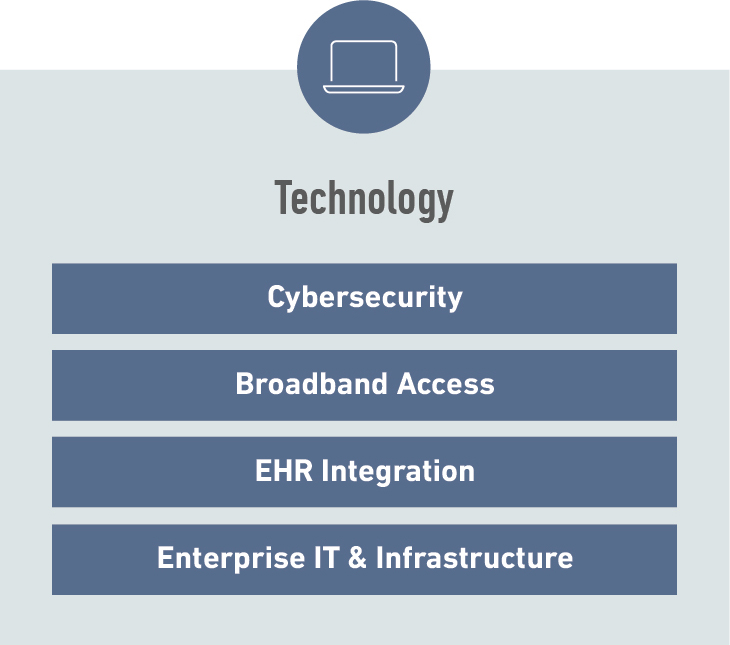
The ability to integrate data and outcomes from telehealth visits with an individual’s broader health record will be critical to providing continued, wholistic, and patient-centered care. With the integration of multiple IT systems and data coming from many sources (e.g., EHR, wearable monitoring devices, telehealth platforms), comes additional cybersecurity challenges that healthcare systems will need to address.
These complexities will continue to plague providers, payers, and patients for years to come – and likely even bring about new challenges related to technology and policy that have been “solved” by the pandemic.
At any point in time, all of these types of challenges – related to Technology, Policy, and Operations – exist in some form. Different healthcare systems will experience these challenges to different degrees, driving diverse approaches to telehealth adoption.
This diversification of challenges brings with it a diversification of opportunities for industry to support healthcare systems – influenced by the unique advantages or disadvantages of each system.
Integrated Delivery Systems: US Government Case Studies
Integrated, risk-bearing delivery systems (especially those with wide geographic distribution of beneficiaries) will likely be the most incentivized to sustain meaningful adoption.
U.S. Government health systems – specifically the Department of Veterans Affairs, the Department of Defense, and Medicaid – and particularly their response to the COVID-19 crisis, provide excellent examples for the future of telehealth and the next wave of challenges and opportunities that will emerge.
Department of Veterans Affairs
The Department of Veterans Affairs has shown to be among the most prominent early movers of telehealth adoption. Its care network has been adopting telehealth solutions since the early 2000s, with more recent programs such as VA Video Connect and the Annie App indicative of advancing technology.
The VA has been uniquely positioned to adopt telehealth due to its extensive infrastructure and service network, allowing the VA to roll out and test programs on a much larger scale than other networks and markets.
Measures taken to mitigate state licensing issues such as the 2018 “Anywhere-to-Anywhere” policy have propelled the VA in terms of utilization by not only expanding patient access but also provider care opportunities.
VA patients have been among the hardest hit by COVID-19 due to age and higher infection rates, seeing nearly 40,000 cases as of July 31, 2020.
To address this rising concern, the VA quickly adopted an “all telehealth” model to ensure that every patient in the VA network still had access to care despite travel restrictions and clinic closures.
During the pandemic, as telehealth became the only option for many veterans, VA smartphone and computer applications saw utilization spike over 1000% during the pandemic.
Weekly VA Video Connect Appointments

Despite previous telehealth programs, many veterans still do not have reliable access to technology at home to benefit from new programs. To address this growing concern, the VA has used funds from the CARES Act to begin distributing tablets equipped with internet connectivity.
In Project ATLAS, the VA partnered with Walmart to set up telehealth kiosks for veterans with limited access to technology at home, illustrating their commitment to finding innovative ways to expand access to virtual care.
When the COVID-19 pandemic eventually subsides, the VA will likely shift its focus towards better integrating telehealth into its existing processes and operations, rather than telehealth simply existing as an adjacent activity – a sign of the VA’s relative maturity in telehealth compared to other systems.
As the VA’s electronic health record modernization continues, integration between its telehealth platforms and the EHR will likely prove necessary. Additionally, as in-person visits begin to return to normal levels, some operational complexity is likely to arise, especially related to scheduling and care delivery.
The VA was an early mover in telehealth, and its unique structural advantages have enabled it to succeed compared to other health systems – but it will still need considerable guidance from the industry as it moves to execute the next phase of post-pandemic telemedicine and a sustainable hybrid model.
Department of Defense
The story of telehealth within the Department of Defense has looked very different. Due to the nature of its continually rotating beneficiary population and global direct care network, the DoD has struggled somewhat to implement a streamlined telehealth system into its care delivery model, beyond historical operational medicine use cases (e.g., battlefield care).
Prior to the pandemic, various telehealth systems existed within the DoD ecosystem. In January 2018, the Army launched its first Virtual Medical Center (VMC) at Brooke Army Medical Center. In the same year, the Navy rolled out Navy Care, a digital health app powered by AmWell piloted at Naval Hospital Jacksonville.
At an enterprise level, the DoD awarded GlobalMed authority to operate on DoD networks in January 2018, making its virtual health care solutions available to all active duty military members and their dependents through the Military Health System.
telehealth implementation at DoD in recent
years, these efforts remain fragmented,
underscoring the complexity of advancing
telehealth from concept to reality."
While there has been significant progress in telehealth implementation at DoD in recent years, these efforts remain fragmented, underscoring the complexity of advancing telehealth from concept to reality.
However, centralization efforts are underway, led by the MHS Virtual Health Clinical Integration Office and establishment of the DHA Virtual Health Program (VHP).
This was reinforced in the FY2021 budget request (released before the pandemic), which requested an additional $10M for the VHP to fund more contractor FTEs, health monitoring platform capabilities, and virtual health synchronous solutions to enable initial operating capability.
Regulation and privacy laws have been a major barrier to large scale telehealth adoption for TRICARE, the civilian care component of the MHS. Previously, TRICARE offered limited reimbursements for telehealth visits and had strict payment requirements for providers outside DoD’s network.
As of May 2020, for as long as the country remains in a state of emergency, TRICARE provides patients access to audio-only telephone visits, waives interstate licensing issues for providers, and waives copayments to encourage telehealth utilization.
COVID-19 has forced the DoD to expand its use of telehealth and put pressure on existing fragmented systems. In addition to TRICARE coverage changes, MTFs transitioned many in-person appointments to virtual visits to make space for coronavirus patients.
The Navy Care program tripled patient enrollment during the pandemic, and provider use of the system increased 104% between February and April 2020.
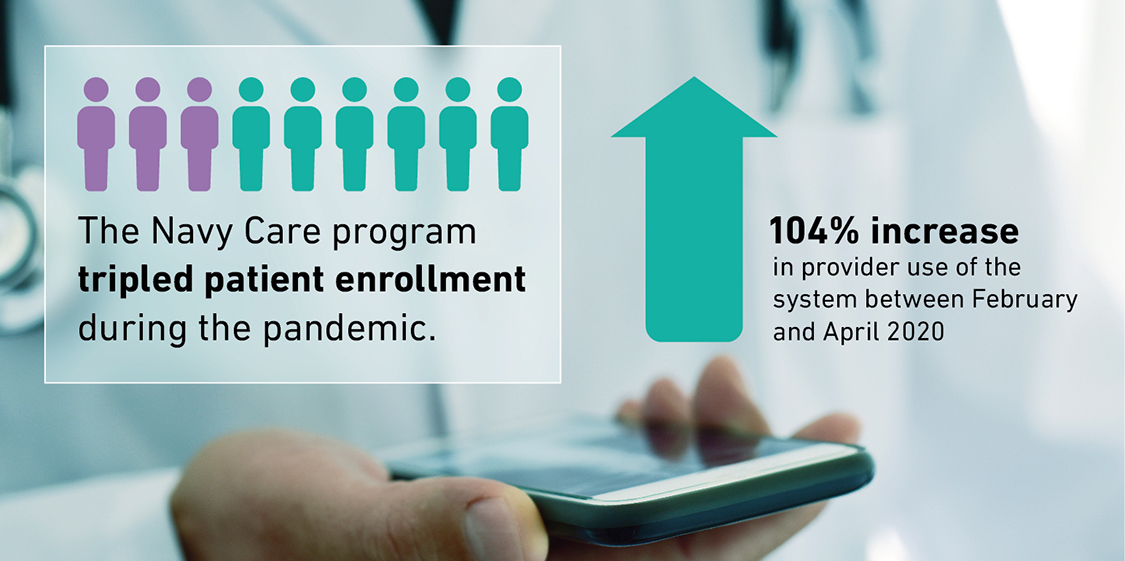
The MHS Nurse Advice Line has seen a dramatic increase in call volume, peaking at more than 10,000 calls in a single day. Created in response to the crisis, the National Emergency Telecritical Care Network (NETCCN) project established a cloud-based standalone health information management system to create virtual critical care wards.
DoD adaptations have been fairly successful, but as the pandemic shows no signs of slowing down, the MHS is likely to evaluate how virtual care can and should play a bigger role in military healthcare moving forward. Draft plans for telehealth expansion from Congress and a new DHA website for telehealth business requests illustrate a promising future for a more centralized DHA-led telehealth system.
But as the DoD matures beyond initial regulatory hurdles at a federal level, its focus will shift toward integration of its telehealth ecosystem as well as increasing patient and provider usage rates.
DHA will see new challenges emerge related to operational execution and technology, especially as it looks to move forward in a consistent, standardized way across its sprawling enterprise.
- How will the DoD sustain momentum for new telehealth efforts while rolling out its new EHR and reorganizing Military Treatment Facilities?
- How will telehealth growth impact future technology requirements in scheduling, revenue cycle management, and other critical systems?
- How will payment parity and changes to TRICARE manifest in future requirements?
Customer stakeholders will look to industry for guidance through this transition period, which will impact not only care delivery but also IT and information management systems, scheduling and operations, claims and payment, and more.
Medicaid
The Centers for Medicare & Medicaid Services work with state providers to ensure that patients are reimbursed for various aspects of care, previously limited to in-person visits.
Historically, the federal Medicaid statute has not recognized telemedicine as a distinct service, hindering widespread adoption.
When COVID-19 began to ravage some U.S. cities in March 2020, restrictive policies surrounding audio-only reimbursement and inter-state licensing issues were relaxed for both Medicare and Medicaid, enabling the rapid escalation of telehealth visits nationwide.
CMS allowed states to apply for waivers to reimburse telehealth visits and allowed providers to operate on a variety of non-HIPPA compliant platforms (e.g., FaceTime, Facebook Messenger) for the duration of the nationwide state of emergency.
Traditional funding hurdles have also been overcome, albeit temporarily, with help from the Families First Coronavirus Response Act (FFCRA) and CARES Act.
These acts increased Medicaid Federal Medicaid Assistance Percentage (FMAP) and allocated money directly to the states to use for Medicaid, helping fund telehealth expenditures during the pandemic.
Some states have acted quickly in the pandemic, breaking down previous barriers to implementation. Massachusetts and Ohio Medicaid systems, both of which had somewhat restrictive reimbursement policies, have loosened restrictions to provide coverage for all telehealth visits and ensure payment parity during the public health emergency.
California and Florida, where telehealth was gaining traction before the pandemic, have expanded Medicaid coverage to include more telehealth devices and services.
New Hampshire has gone the furthest to ensure the changes ushered in by the pandemic outlast the crisis, enacting a new law in July 2020 that requires Medicaid and private payers to reimburse telehealth services on the same basis as in-person care.
These actions have been taken during a nationwide state of emergency, but the longevity of the impact on state Medicaid policy is still to be determined.
The pandemic has demonstrated how telehealth has been successful as a short-term solution for minimizing COVID transmission risk.
will necessarily focus on cost effectiveness,
including potentially eliminating payment parity,
with demonstration of efficacy taking center stage"
Thus, post-COVID state Medicaid telehealth policies will necessarily focus on cost effectiveness, including potentially eliminating payment parity, with demonstration of efficacy taking center stage.
As widespread telehealth adoption is still relatively immature, the empirical evidence linking utilization with improved clinical outcomes and reduced costs is lacking.
State leaders will look to industry for data analysis, advisory support, and other activities to determine the long-term viability of telehealth as a critical part of Medicaid.
Beyond the Crisis: Considerations for Industry
While the pandemic has prompted forward progress at an unprecedented pace, these case studies illustrate the many challenges health systems still need to navigate and that long-lasting, widespread telehealth adoption is only just beginning.
Collaboration with and innovation from industry across many areas – technology, policy, and operations – will be essential as we transition to post-pandemic meaningful adoption and look to “get off the starting line.”
Companies working with government are in a unique position to drive this innovation and forward progress, both in and beyond technology.
Potential Solutions to the Challenges Emerging from Telehealth
- How do I differentiate in an increasingly crowded market?
- What technology challenges have emerged due to the growing maturity of telehealth across government systems?
- What questions do my clients have – and how can I position to help answer those questions?
- How do we measure and evaluate success?
- How do we incentivize adoption and disseminate best practices?

- How can I rethink my current solutions and operations to incorporate telehealth?
- How can I help my customers design and implement a sustainable, integrated care delivery model that includes telehealth?
Federal contractors looking to get involved should consider the following actions:
-
- Help your customers design something sustainable for the future.
How can they address the new challenges emerging in the next phase of telehealth adoption – both from a policy and operational perspective? How do they measure and evaluate success? What successes and lessons learned can we take from government “early adopters” and apply as best practice across other health systems? - Re-think your own operations.
How can telehealth become a natural part of your current portfolio? How might your current business operations need to change to adapt to widespread telehealth adoption? How might a new operational model enable telehealth applications to your current service provision? - Find ways to differentiate.
As every digital company scrambles to capture the resulting spending increase due to broader telehealth adoption, Federal services firms will need to find ways to differentiate from the crowd and provide a new solution – whether it’s a telehealth platform or a solution supporting related processes and activities.
- Help your customers design something sustainable for the future.
As firms consider how to adapt, where to invest, and who to engage as we enter this new phase of adoption, Avascent can support firms in a variety of capacities.
In a time of uncertainty, an external, market-based perspective in determining the highest return-on-investment areas and developing a strategy for the future is essential.
We welcome your questions and dialogue around your firm’s experience in the market and ways to address future challenges as our healthcare systems enter a new phase of care delivery.





